Prostate Cancer: What you Need to Know
Prostate cancer is when cancer forms in the prostate gland. It is the second-leading cause of cancer deaths for men in the U.S. About 1 in 9 men will be diagnosed with prostate cancer in their lifetime. This year, nearly 165,000 men will be diagnosed with prostate cancer.
Growths in the prostate can be benign (not cancer) or malignant (cancer).
Benign growths (like benign prostatic hypertrophy (BPH):
- Are rarely a threat to life
- Don’t invade the tissues around them
- Don’t spread to other parts of the body
- Can be removed and can grow back very slowly (but usually don’t grow back)
Malignant growths (prostate cancer):
- May sometimes be a threat to life
- Can infect nearby organs and tissues (such as the bladder or rectum)
- Can spread (metastasize) to other parts of the body (like lymph nodes or bone)
- Often can be removed but sometimes grow back
Prostate cancer cells can spread by breaking away from a prostate tumor. They can travel through blood vessels or lymph nodes to reach other parts of the body. After spreading, cancer cells may attach to other tissues and grow to form new tumors, causing damage where they land.
When prostate cancer spreads from its original place to another part of the body, the new tumor has the same kind of abnormal cells and the same name as the primary (original) tumor. For example, if prostate cancer spreads to the bones, the cancer cells in the bones are actually prostate cancer cells. The disease is metastatic prostate cancer, not bone cancer. For that reason, it’s treated as prostate cancer in bone.
To understand prostate cancer, it helps to know how the prostate normally works.
THE PROSTATE
The prostate and seminal vesicles are part of the male reproductive system. The prostate is about the size of a walnut and weighs about one ounce. The seminal vesicles are two much smaller paired glands. These glands are attached to each side of the prostate. The prostate is below the bladder and in front of the rectum. It goes all the way around the urethra. The urethra is a tube that carries urine from the bladder out through the penis.
The main job of the prostate and seminal vesicles is to make fluid for semen. During ejaculation, sperm is made in the testicles, and then moves to the urethra. At the same time, fluid from the prostate and the seminal vesicles also moves into the urethra. This mixture-semen-goes through the urethra and out of the penis as ejaculate.
When cancer occurs, it is found in the prostate gland and almost never in the seminal vesicles.
SCREENING
“Screening” means testing for a disease even if you have no symptoms. The prostate specific antigen (PSA) blood test and digital rectal examination (DRE) are two tests that are used to screen for prostate cancer. Both are used to detect cancer early. However, these tests are not perfect. Abnormal results with either test may be due to benign prostatic enlargement (BPH) rather than cancer.
The American Urological Association (AUA) recommends talking with your healthcare provider about whether or not you should be screened. To find out if prostate cancer screening is a good idea, take our Know Your Stats Risk Assessment Test. Tell your results to your healthcare provider when you talk about the benefits and risks of screening.
The two main types of screenings are:
PSA BLOOD TEST
The prostate-specific antigen (PSA) blood test is one way to screen for prostate cancer. This blood test measures the level of PSA in the blood. PSA is a protein made only by the prostate and a prostate cancer. The test can be done in a lab, hospital or healthcare provider’s office.
Very little PSA is found in the blood of a man with a healthy prostate. A low PSA is a sign of prostate health. A rapid rise in PSA may be a sign that something is wrong. Prostate cancer is the most serious cause of a high PSA result. Another reason for a high PSA can be benign (non-cancer) enlargement of the prostate. Prostatitis, inflammation of the prostate, can also cause high PSA results.
A rise in PSA level does not tell us the type of cancer cells present. The rise tells us that cancer may be present.
Talk with your healthcare provider about whether the PSA test is useful for you. If you decide to get tested, be sure to talk about changes in your PSA score with your provider. Make sure to watch our video on the PSA Blood test.
DIGITAL RECTAL EXAM (DRE)
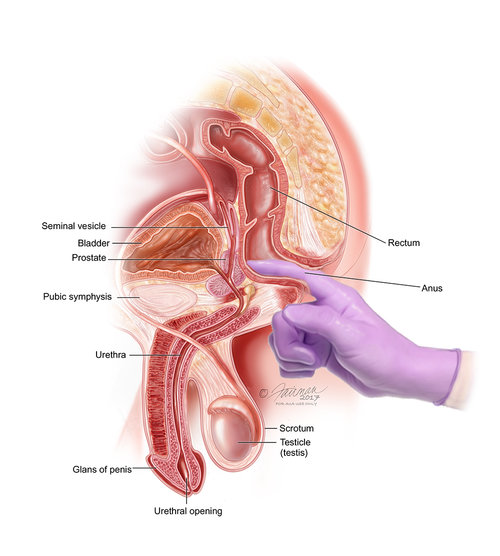
The digital rectal examination (DRE) helps your doctor find prostate problems. For this exam, the healthcare provider puts a lubricated gloved finger into the rectum. The man either bends over or lies curled on his side on a table. During this test, the doctor feels for an abnormal shape or thickness to the prostate. DRE is safe and easy to do. But the DRE by itself cannot detect early cancer. It should be done with a PSA test.
WHO SHOULD GET SCREENED?
Screening is recommended if you are a man:
- Between 55–69 years old
- African–American
- Have a family history of prostate cancer
WHAT ARE THE BENEFITS AND RISKS OF SCREENING?
The PSA test and DRE are very important tools. They help to find prostate cancer early, before it spreads. When found early, it can be treated early which helps stop or slow the spread of cancer. This is likely to help some men live longer.
A risk of a PSA test is that it may miss detecting cancer (a “false negative”). Or, the test may be a “false positive,” suggesting something is wrong when you are actually healthy. A false positive result may lead to a biopsy that isn’t needed. The test might also detect very slow growing cancer that will never cause problems if left untreated.
WHAT IS A BIOPSY?
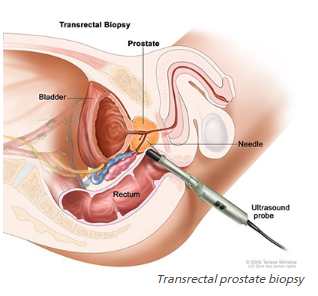
Transrectal prostate biopsy
A Biopsy is a type of surgery. For a prostate biopsy, tiny pieces of tissue are removed from the prostate and looked at under a microscope. The pathologist is the doctor who will look carefully at the tissue samples to look for cancer cells. This is the only way to know for sure if you have prostate cancer.
The decision to have a biopsy is based on PSA and DRE results. Your doctor will also consider your family history of prostate cancer, ethnicity, biopsy history and other health factors.
Prostate biopsy is best done with ultrasound and a probe. You may be given an enema and antibiotics to prevent infection. For the test, you will lie on your side as the probe goes into the rectum. First, your provider takes a picture of the prostate using ultrasound. Your healthcare provider will note the prostate gland’s size, shape and any abnormalities. He/she will also look for shadows, which might signal cancer. Not all prostate cancers can be seen, and not all shadows are cancer. The prostate gland is then numbed (anesthetized) with a needle passed through the probe. Then, the provider removes a very small piece of your prostate. The amount of tissue removed depends on the size of the gland, PSA results and past biopsies.
Make sure to watch our video on Prostate Cancer Biopsy.
If cancer cells are found, the pathologist will assign a “Gleason Score” which helps to determine the severity/risk of the disease (see Stages for more information).
After a biopsy, you may have blood in your ejaculate, urine and stool. This should go away fairly quickly. If not, or you get a fever, contact your doctor.
HOW IS PROSTATE CANCER GRADED AND STAGED?
Grading (with the Gleason Score) and staging defines the progress of cancer and whether it has spread:
GRADING
When prostate cancer cells are found in tissue from the core biopsies, the pathologist “grades” it. The grade is a measure of how quickly the cells are likely to grow and spread (how aggressive it is).
The most common grading system is called the Gleason grading system. With this system, each tissue piece is given a grade between three (3) and five (5). A grade of less than three (3) means the tissue is close to normal. A grade of three (3) suggests a slow growing tumor. A high grade of five (5) indicates a highly aggressive, high-risk form of prostate cancer.
The Gleason system then develops a “score” by combing the two most common grades found in biopsy samples. For example, a score of grades 3 + 3=6 suggests a slow growing cancer. The highest score of grades 5+5=10 means that cancer is present and extremely aggressive.
The Gleason score will help your doctor understand if the cancer is as a low-, intermediate- or high-risk disease. Generally, Gleason scores of 6 are treated as low risk cancers. Gleason scores of around 7 are treated as intermediate level cancers. Gleason scores of 8 and above are treated as high-risk cancers.
If you are diagnosed with prostate cancer, ask about your Gleason score and how it impacts your treatment decisions.
STAGING
Tumor stage is also measured. Staging describes where the cancer is within the prostate, how extensive it is, and if it has spread to other parts of the body. One can have low stage cancer that is very high risk. Staging the cancer is done by DRE and special imaging studies.
The system used for tumor staging is the TNM system. TNM stands for Tumor, Nodes and Metastasis. The “T” stage is found by DRE and other imaging tests such as ultrasound scan, CT scan, MRI scan. The imaging tests show if and where the cancer has spread, for example: to lymph nodes or bone.
These staging imaging tests are generally done for men with a Gleason grade of 7 or higher and a PSA higher than 10. Sometimes follow-up images are needed to evaluate changes seen on the bone scan.
IMAGING TESTS
Not all men need imaging tests. Your doctor may recommend imaging exams based on results from other tests.
Prostate cancer may spread from the prostate into other tissues. It may spread to the nearby seminal vesicles, the bladder, or further to the lymph nodes and the bones. Rarely, it spreads to the lungs and or other organs.
Your healthcare provider may recommend a pelvic CT scan , an MRI scan or a bone scan to check if your cancer has spread.
WHAT ARE THE SURVIVAL RATES FOR PROSTATE CANCER?
Many men with prostate cancer will not die from it; they will die from other causes. For men who are diagnosed, it is better if it is caught early.
Survival rates for men with prostate cancer have increased over the years, thanks to better screening and treatment options. Today, 99% of men with prostate cancer will live for at least 5 years after diagnosis. Many men having treatment are cured. Most prostate cancer is slow-growing and takes many years to progress. One out of three men will survive after five years, even if the cancer has spread to other parts of the body.
Treatment
Some cancers grow so slowly that treatment may not be needed at all. Others grow fast and are life-threatening so treatment is usually necessary. Deciding what treatment you should get can be complex. Talk with your healthcare team about your options. Your treatment plan will depend on:
- The stage and grade of the cancer (Gleason score and TNM stage)
- Your risk category (whether the cancer is low, intermediate or high risk)
- Your age and health
- Your preferences with respect to side effects, long-term effects and treatment goals
Results from other diagnostic tests will help your provider understand if the cancer can spread or recur (return) after treatment.
Before you decide what to do, you should consider how immediate and long-term side effects from treatment will affect your life, and what you’re willing to tolerate. Also, you should consider that you may try different things over time.
If you have time before you start treatment, consider your range of options. Get a second opinion from different prostate cancer experts. You may need to see another urologist, oncologist or radiation oncologist. Consider the expertise of your doctor before you begin. With more experienced surgeons, the risk of permanent side effects (like incontinence) is lower. Also, it helps to talk with other survivors and learn from their experiences.
In addition, try and get or stay healthy. Eating a well-balanced diet, maintaining a healthy weight, exercising and not smoking are all important factors when fighting prostate cancer..
Moreover, don’t ignore your emotions. Think about how you’re coping with this diagnosis. Many men who have prostate cancer feel worried, stressed and angry. You and those that care about you may need to consider professional counseling.
Treatment choices for prostate cancer include:

